World Breastfeeding Week: Hope & Frustration
Categories: babies, bottlefeeding, breastfeeding & lactation, feeding babies & kids, postpartum, pumping, toddlers & older kidsAugust 7, 2016
author: Jeanette Mesite Frem
It was World Breastfeeding Week last week.
World Breastfeeding Week was created to encourage global organizations and community organizations work together to improve sustainable development through the protection, promotion and support of breastfeeding. I meant to post something last week but got busy helping babies with breastfeeding and watching and reading of all the posts and memes related to WBW that came across my Facebook timeline. I found inspirational messages of hope and progress. I found articles that frustrated me about how people need to cover up when nursing or how health insurance companies are working hard to deny coverage of lactation support despite the Affordable Care Act requiring coverage.
Why do we need a week devoted to breastfeeding? Because we have hope. And because there's so much more work to be done. And because breastfeeding (and not breastfeeding) affects so many aspects of life: nutrition, food security, poverty reduction, survival, health and wellbeing, environment and climate change, women’s productivity and employment, sustainable partnership and the rule of law.
Yep, drops of milk don't only affect each person but drops of milk can affect life on a global level. There's a link at the bottom of this post which will help you find out more about the 2016 World Breastfeeding Week and fascinating details about the many factors just mentioned.
Did you know that despite global health recommendations for infants to be breastfed exclusively for the first six months of their lives, less than 40% of infants are exclusively breastfed, and only 20% in Massachusetts. Yeah, let's talk about frustration.
It’s interesting to look at the data. [Edited to update with 2016 numbers] The 2016 CDC data for Massachusetts shows:
- 87.4% of babies are ever breastfed (which means baby latched on at least once before hospital discharge or mom says she plans to breastfeed after discharge)
- But then numbers drop severely…67.9% of babies are breastfeeding at all at 6 months
- Only 38.7% at are still breastfeeding at all by 1 year (by the way, the US is the only country in the world that sets 1 year as a goal instead of the global standard of two years)
- Then if you look at exclusively breastfed until 6 months, that number is only 19.9%.
So, wait. Let's really think about these numbers. While they are higher than they were in the 2014 CDC report, they still aren't that great, considering global recommendations and the impact of breastfeeding on health for parents and babies.
EIGHTY-ONE PERCENT of moms start out WANTING to breastfeed but only TWENTY-FIVE PERCENT make it to 1 year?
And the globally agreed-upon standard (biologically) is that babies are supposed to be exclusively breastfed until SIX MONTHS but only SEVENTEEN PERCENT of Massachusetts babies get that?
WHAT IS HAPPENING HERE??
LACK OF PROFESSIONAL EDUCATION
Can you imagine if the statistic was about WALKING...another BIOLOGICALLY NORMAL aspect of life. Imagine your baby was born and you had expectations that he would walk by a year. And he didn't show any signs of walking. Would it be okay if your baby's doctor and everyone else around you just said, "it's okay, just give the kid a wheelchair...he'll still be able to get around." No, of course not. But if your baby is struggling with nursing and someone tells you "just give him a bottle"...that may be a temporary solution, but that isn't fixing the original problem, now, is it?
I feel like this is what I hear from parents all the time. "I wanted to avoid formula but the pediatrician told me that formula was better." I heard from one mom recently that she actually asked the doctor if she could pump and give her milk instead and the pediatrician allegedly said, "No, I'd prefer you use formula."
Another set of parents (TWO witnesses!) told me recently that they were offered a choice between donor milk and formula in the hospital. They weren't sure what to do as they didn't know anything about donor milk (which is sad that no one had prepared them for that prenatally!). They asked the nurse "what would you do?" and she allegedly said "I'd go with the formula, you never know what you are getting in the donor milk." Whoa. It's 2016 people. That's just incorrect. Screened and pasteurized donor milk comes from the milk bank near Boston. We know a LOT about what is in it. When donor milk is available, it should always be the first choice.
Can we get some education to these health professionals? Did you know that nurses and doctors have little training in breastfeeding and the science behind human milk? Some do, don't get me wrong...I have many medical professionals who are my go-to people when I have questions about my clients. I have a long list of beloved and respected MDs, NPs, PAs, RNs, OTs, PTs, SLPs who I know support breastfeeding and human milk feeding whenever possible. But over all, there's a dearth of education in our medical system. It's not going to change unless parents demand it. You are the consumers. Be heard.
Now before you have your hairs raise on your neck and your heart starts beating faster, I'm NOT talking here about folks who don't want to breastfeed or parents who literally don't make enough milk for their babies. I'm NOT talking about babies who have complex medical situations that make it crazy-difficult to suck and swallow. Then again, there are PLENTY of folks who don't get help to find out if they COULD make more milk or if baby COULD actually latch with some simple (or complex but effective) adjustments or procedures. I've met many of those who DO find help and they are thrilled they got that help even if it helped baby nurse one more time or drink formula at the breast through a tube or have one more ounce of their own milk each day. But wow, those parents work harder than anyone else to make those drops of milk or get those babies to latch well. They are the reason behind why I do what I do in my work as a lactation consultant and prenatal breastfeeding educator. Those families are the main inspiration.
HEAVY MARKETING INFANT FORMULA
Before you left the hospital, were you given information about the support available to you in your community around breastfeeding? Probably not. Unfortunately, many of the reasons that babies aren’t breastfed pertain to parents not having the support they need at the time they need it AND the fact that there is aggressive marketing of infant formula.
It's a MULTI-BILLION dollar industry. Even in our area hospitals (where pasteurized donor milk is available and not all babies receiving formula actually need it). Here's an interesting fact. When a formula representative visits a pediatrician's office, they are welcomed and hold meetings with them to learn more about their product, a pharmaceutical product. They are given free samples which are then given for free to families. [Again, I totally understand the need for doctors to have this stuff on hand, both in the hospital and clinics.]
But I bet you heard about formula and might have even been given some by a nurse or doctor within the first week of your baby's life, EVEN IF you were making enough milk. I bet you received formula in the mail before your baby arrived (thanks for that goes to your baby registry stores or your OB's office for giving them your address, by the way). Did you know that having formula in the house increases the risk of quitting breastfeeding quickly? Fortunately, in Massachusetts, there was a law passed banning formula-filled "breastfeeding support bags" given out by hospitals (provided for free to the hospitals by formula companies, who give hundreds of thousands of dollars to hospitals to market their products and give out free samples). However, if a parent is convinced their baby needs formula (even though mom could start pumping) or if a parent asks for formula, they are given the bag of free samples anyway. I could go on. But I'll move on from this specific piece by saying that fortunately SOME hospitals in Massachusetts are working toward an international "baby-friendly" designation which should greatly help, but some big birthing hospitals aren't even making an effort. Sad.
LIMITED ACCESS TO LACTATION CARE PROFESSIONALS
So, do you think hospitals are helping to spread the word about the services provided by area breastfeeding supporters and IBCLCs? Think again.
When an IBCLC-lactation consultant like myself tries to get a meeting with a doctor to let them know about my services, we are usually unable to get past the front desk, and they aren't even happy to take business cards or flyers. Sometimes I get a smile. Sometimes I'm told "we already have someone we refer to." Okay, so having one option is all your clients need or want? Sometimes I'm told they "aren't allowed to take marketing materials" despite all the ads for drugs I see in their waiting room. One would think they'd be happy to find out about services and groups (and prenatal classes) they can tell their clients about. Unfortunately, it's not usually the case.
LACK OF REFERRALS TO COMMUNITY SUPPORT GROUPS
The World Health Organization and the United Nations Children’s Fund created the Ten Steps to Successful Breastfeeding and that the Tenth Step is “Foster the establishment of breastfeeding support groups and refer mothers to them on discharge from the hospital or clinic.” Did your birthplace refer you to any support groups in your community? Did you know (cough, ahem, cough, cough) that there are typically 2 groups per week (sometimes three!) at this place called Babies in Common…did you hear about the groups here from your birthplace or baby's doctor? Probably not. If you did, PLEASE let me know! ;)
Ooh, oooh, ooh...by the way, I JUST found out that one large local hospital took Babies in Common AND all other local groups OFF of its list of community resources. What’s up with that?!
Have your baby’s doctors told you about the community support available here or elsewhere? Speaking of, what ARE the other options near you? You can ask me. I know about some of them. Or, as apparently the hospitals want you to do in your tired and postpartum emotional state, you can search online. Look on zipmilk.org for info on finding other IBCLCs and support groups in your area. It’s totally OKAY to attend MORE than one breastfeeding group per week (“breastfeeding” also includes pumping, chestfeeding!). One of the moms who attends groups at BinC also goes to two other groups. That’s some dedicated driving but she meets a lot of different people and learns a lot of things. Also, there is a moms’ group and parents' group here at Babies in Common led by social worker Jill Vetstein…these groups are NOT about feeding but about everything else! :)
What can YOU do to help all the parents and babies in the future get more support?
WRITE to the President of your birthplace, the charge nurse of the maternity unit, your obstetrical care provider and your baby’s doctor’s office and ask them, “Why didn’t you tell me about Babies in Common or other options near me?” Tell them your story. The more letters they receive, the more changes may happen. Squeaky wheel gets the oil, ya know. Hey, one more thing. Write to some of the folks at the Commissioner's office at the MA Department of Public Health. Here's a link.
Do you know who the breastfeeding helpers are?
There are several different types of breastfeeding helpers. Experienced moms. Nurses. Midwives. Possibly doctors. Free community peer counselors. La Leche League Leaders and groups. Nursing Mothers' Counselors (I used to be one). Breastfeeding counselors and lactation educators who go by different certifications. Unfortunately, parents aren't informed of the differences.
Unfortunately, most families AND most doctors don’t know the difference. Often I hear someone say, “my pediatrician’s office has a lactation consultant” when that person is actually a well-meaning nurse who took a one-week training. That’s wonderful and may be just what some babies need but that's not the same as what an IBCLC can do for you. Just be informed and be careful. If you are having issues that a friend or a doctor or a breastfeeding counselor can’t help you with, seek out an IBCLC, the gold standard in lactation care. If she doesn't help you, find another one. Second opinions are important.
Also look at where they work. Hospital and clinic-based IBCLCs sometimes have limitations on their time or what they are allowed to tell you (compared to private practice IBCLCs like me). Hear these two things:
- there are actually hospitals that will reprimand or fire anyone on their lactation staff that discusses tongue tie or lip tie with parents of a new baby. Really. It's true. I've heard of from many of my colleagues.
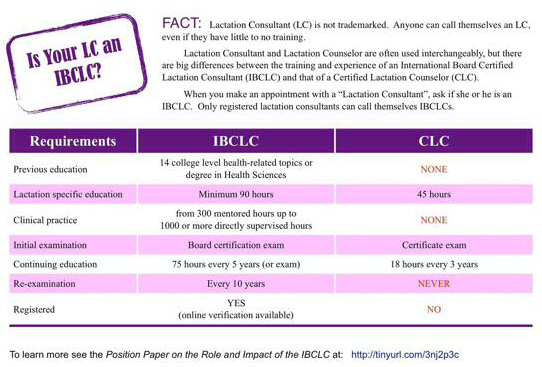
- there's actually a movement in in the US working toward equating lactation counselors (a needed group of people, of course!) with International Board Certified Lactation Consultants (IBCLC), who have MUCH more formal training and clinical experience (and who take an international board exam that is given by an independent organization). See below for a graphic showing the differences between the two professionals. We need both, but they are not equal.
Even the Centers for Disease Control is confusing things with its recent report which seems to equate the two. Breastfeeding counselors (particularly those called CLCs, Certified Lactation Counselors) have one week of training. One week. I was once at that level and that amount of training, along with my experiences nursing my own kids and helping families along the way as a birth doula, allowed me to help many families with simple questions or positioning suggestions but when there were issues…I referred to an IBCLC. Because they have the training and experience to work with those with simple AND complex issues.
What's wrong with one week of training, you might be wondering. Does that sound good enough to you when you have mastitis, nipples that are bleeding, a baby that is too skinny, pumping sessions which yield only 1/4 of an ounce or less?
Think about it this way. Medical assistants are important parts of the medical team. They have one YEAR of formal training. They can't be hired to weigh you and take your vital signs after one week of training. They don't walk around saying they are doctors, now, do they? So, how can one WEEK of training prepare someone to help with the complexities of the breast as an organ, the breastfeeding dyad of parent and baby, the complications that arise from breast infections, shredded nipples and low milk supply? It simply can't.
Now, I'm NOT equating the IBCLC with an MD, either, here, but when it comes to breastfeeding and lactation, IBCLCs ARE the people who have the MOST training in breastfeeding and lactation. There are a FEW physicians who have passed the IBCLC exam and now practice as breastfeeding medicine doctors, but we have exactly ONE in Massachusetts. Sad, but true. And even she only sees clients 1-2 days per week. Some states have zero breastfeeding medicine doctors. But how many IBCLCs are in private practice in Massachusetts? THIRTY, according to my recent search on the International Lactation Consultant Association's website. And NOT all 30 of us are busy. MassHealth doesn't cover our services. And we all hear this far too often, "if I had know about you when my baby was first born, I might have kept on breastfeeding." We are available. And some of us, after all our training, end up retiring because we can't make a living from providing lactation support. It would help if we were given a license by the state. Only TWO states in the country have licensing. It's so odd. The gold standard internationally and in the US for lactation care and yet we're not state licensed as allied health professionals. There's a team working on that in Massachusetts. Consider helping with their efforts by clicking here to learn how.
Yeah, that's what's missing: Parents with new babies are NOT getting the information about the support available to them. I'm sorry for that. I'm working to spread the word. But YOUR VOICE needs to be heard.
If you wish that you knew about my services, the support groups at Babies in Common, the other support groups you found or the IBCLC you found who helped you, then CALL your doctor or midwife and tell them. WRITE to the head of your birthing hospital (and the charge nurse and the head of obstetrics and the head of pediatrics) and tell them they should have told you. Maybe use the hashtag #youshouldhavetoldme ??
Most major changes that happen in the world start with one person. Be one.
Thanks for reading.
Click here to find out more about World Alliance for Breastfeeding Action
Click here to learn more about the Massachusetts Breastfeeding Coalition (MBC)
Click on the graphic above to see a larger view (this will open a new page in your browser).